30 Hospital Discharge Summary Templates (& Examples)
of entry to discharge How to write progress notes How to use the PT's initial examinations, evaluations, and plan of care when writing progress notes Legal matters related to documentation Reimbursement basics and documentation requirements The text also contains a section titled SOAP Notes Across the Curriculum, or SNAC. This section provides
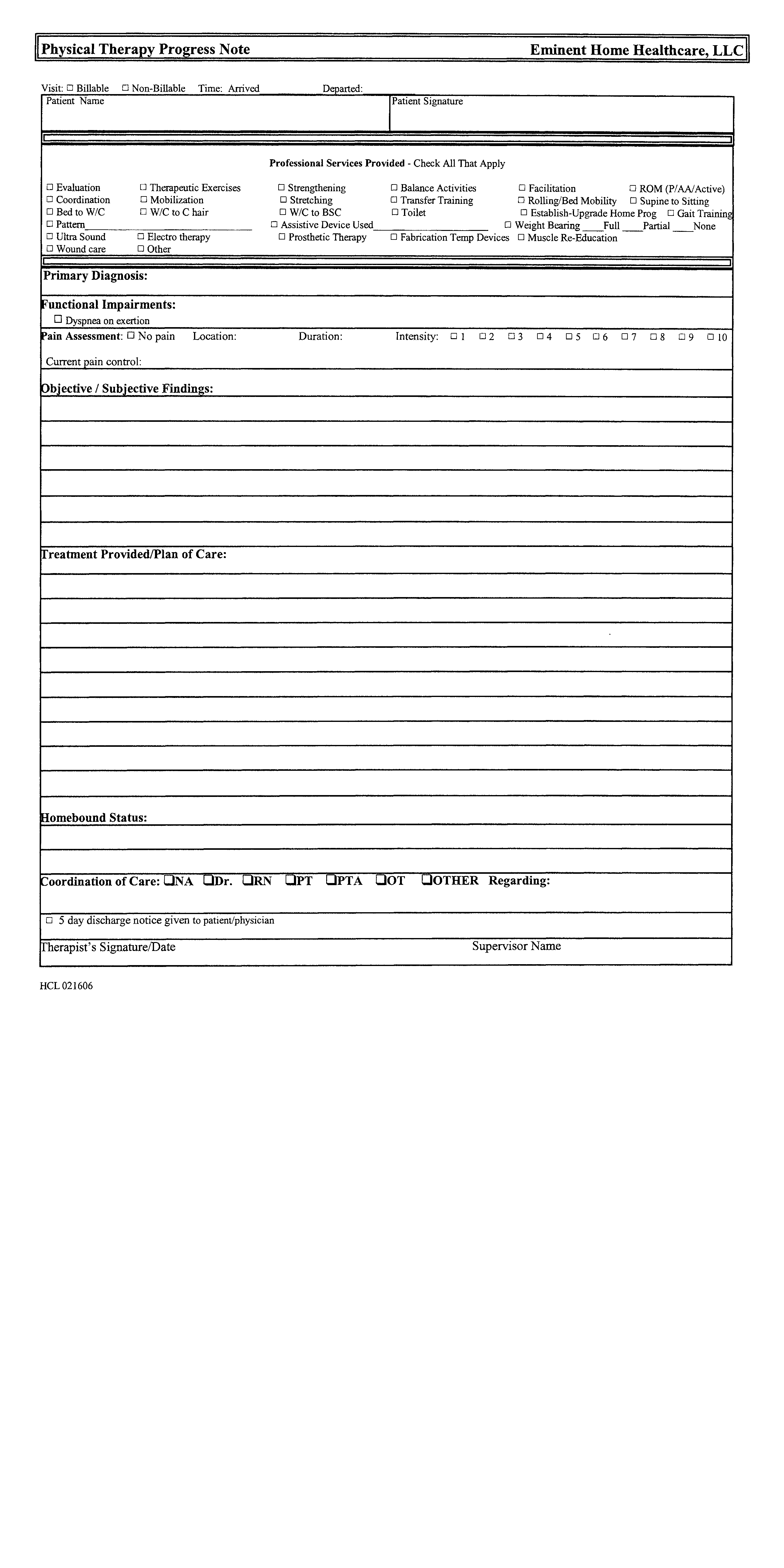
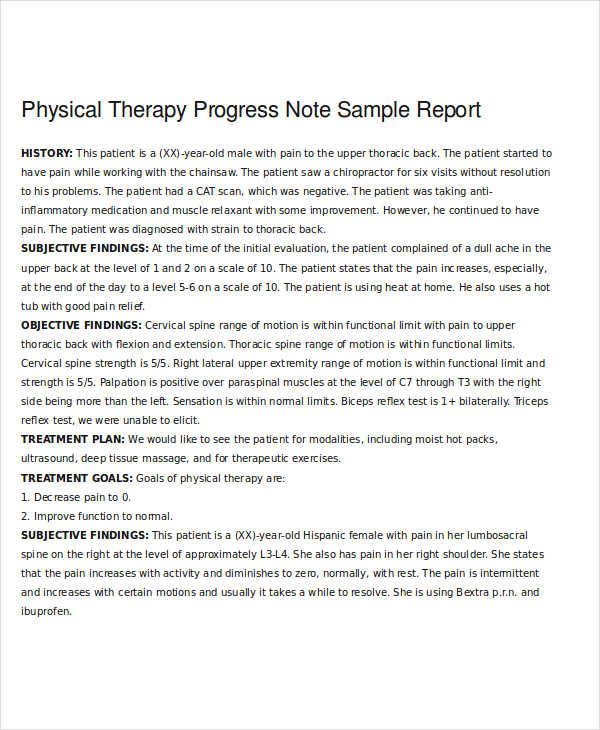
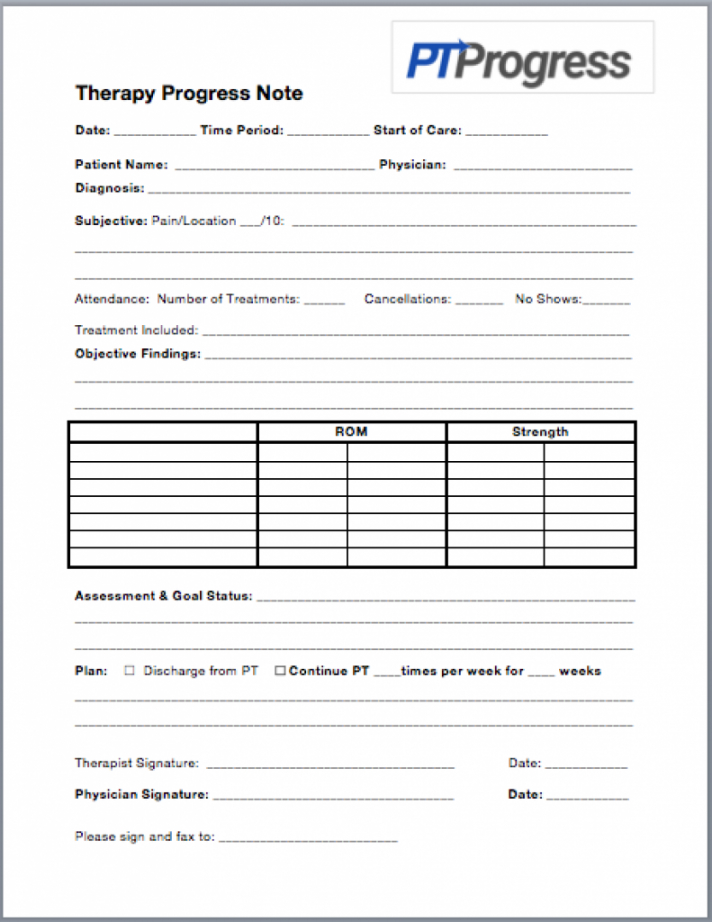
Therapy Progress Notes Template
A discharge summary is a version of a progress report. Progress reports do not require a physician or non-physician practitioner's signature unless it functions as an update to the plan of care, significantly change the plan of care, or is required to update or recertify the plan of care. Sample Physical Therapy Progress Report Checklist:
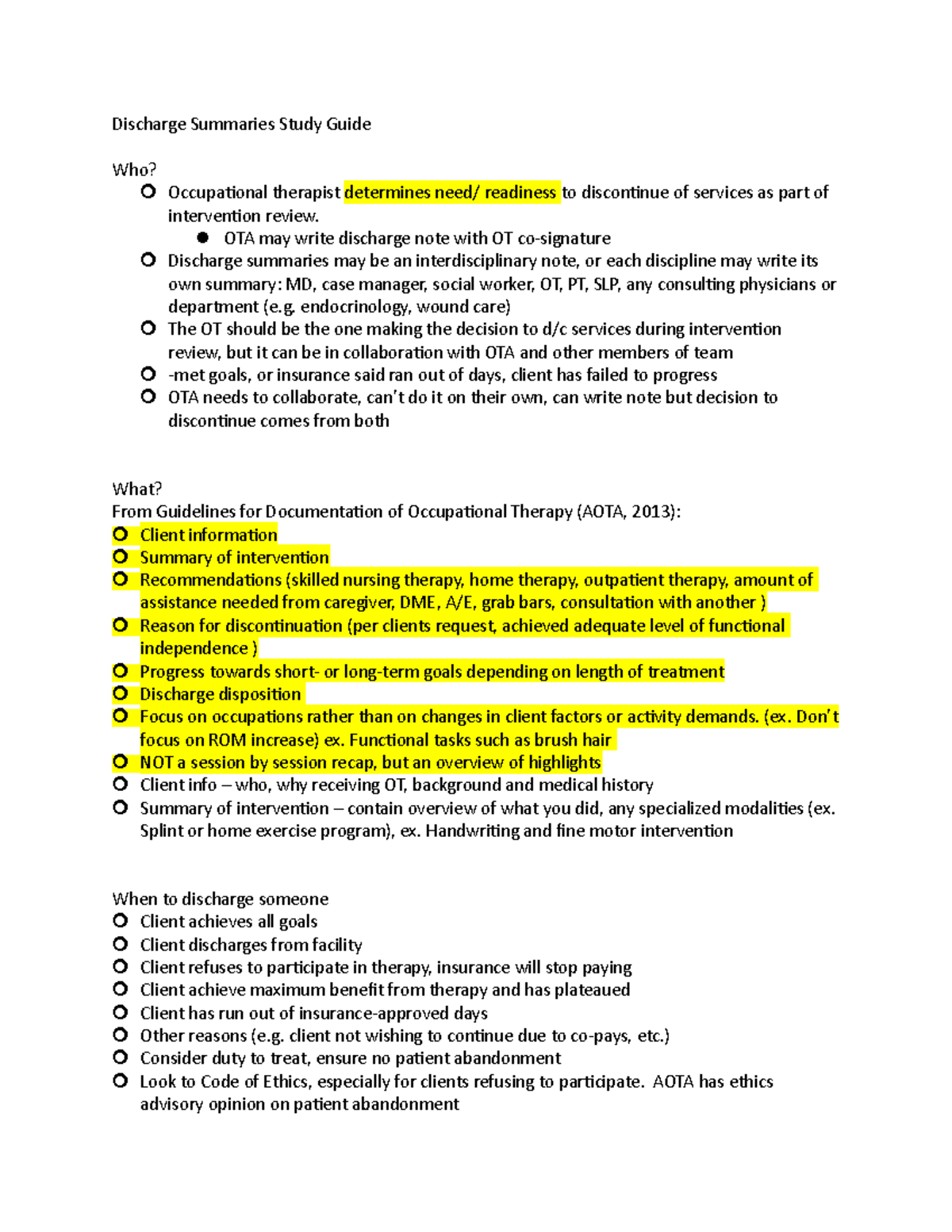
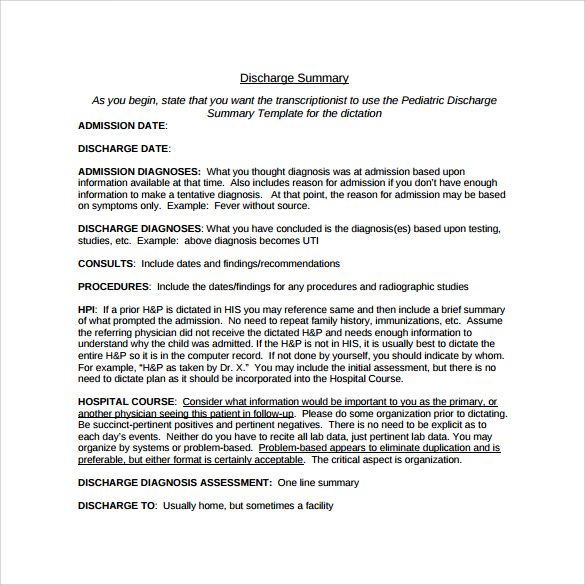
Discharge Summaries Study Guide Discharge Summaries Study Guide Who
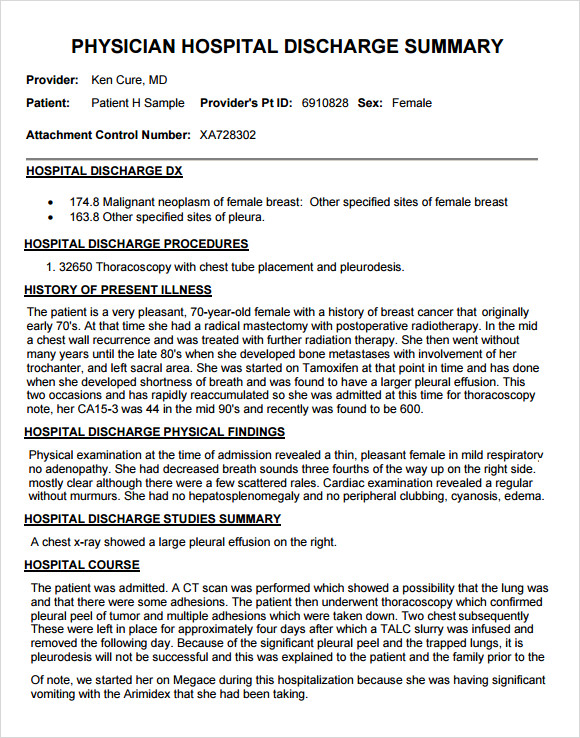
A discharge summary is a clinical report prepared by a health professional at the conclusion of a hospital stay or series of treatments. It is often the primary mode of communication between the hospital care team and aftercare providers. It is considered a legal document and it has the potential to jeopardize the patient's care if errors are.
FREE 7+ Sample Discharge Summary Templates in PDF MS Word
In keeping with SOAP, a progress note typically includes the following: Subjective and Summary of Treatments Provided. Objective: ROM, strength, special tests. Assessment and Goal Status. Plan and Recommendation. When writing a progress note, understand that the physician may have less than a minute to review your notes.

How To Write Therapy Progress Notes 8 Templates & Examples
WebPT is here to help you understand and tackle how to write Physical Therapy Progress Notes and Discharge Summaries. PXM. PXM Overview. One interconnected platform that catapults your practice into the future with solutions to engage patients, drive satisfaction, and accelerate financial growth.
FREE 11+ Sample Discharge Summary Templates in PDF MS Word
PROGNOSIS: Pt. has excellent potential to meet expected outcomes of therapy due to his excellent motivation to return to work, young age, no prior injury to the ® shoulder, & overall good physical conditioning prior to injury. Expected to progress to being able to successfully & safely complete light duty tasks for work in 3 wks & return to.
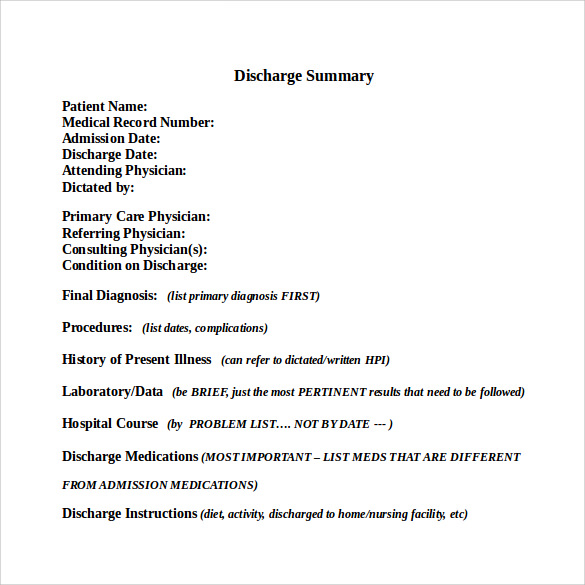
FREE 11+ Sample Discharge Summary Templates in PDF MS Word
The minimal requirements for a Medicare physical therapy progress note for Part B outpatient services. References and links are available at http://www.phys.

Physical Therapy Note Template & Example Free PDF Download
A physical therapy progress note is a legal document written by a professional occupational therapist. The aim of a note is to track a patient's care process, write prescriptions, document complaints, and outline treatment plans. Clinicians employ the instrument of note-taking to get the most out of the planning process.
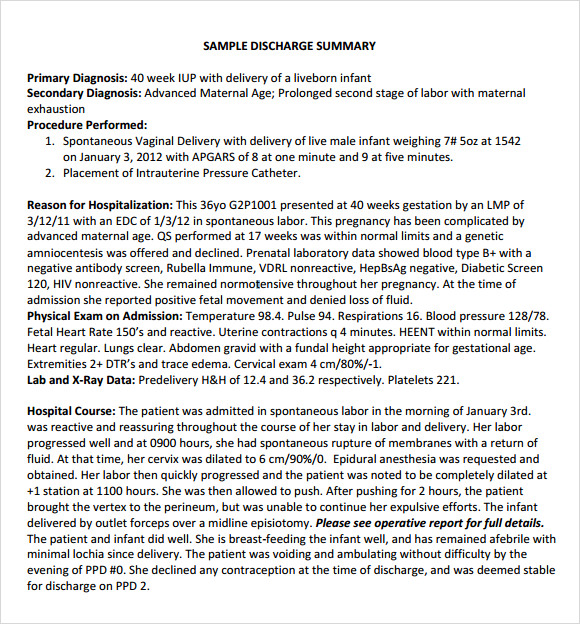
FREE 7+ Sample Discharge Summary Templates in PDF MS Word
WebPT is here to get you understand and tackle how to record Physical Cure Progress Notations and Discharge Summaries
Progress Note 18+ Examples, Format, Pdf Examples
A discharge note, also called a termination note, is a written summary held in the client's chart of what happened during the time the client was in your care. A progress note typically uses a SOAP or GIRP format and documents weekly sessions. A discharge note, on the other hand, spans a broader amount of time and gives a high-level view of.

Free Printable Discharge Summary Templates [Word, PDF] / Mental Health
Ability to assume or resume work (job/school/plan), community, and leisure activities with or without assistive, adaptive, orthotic, protective, supportive, or prosthetic devices and equipment. Ability to gain access to work (job/school/play), community, and leisure environments.
Free How To Write A Progress Note Physical Therapy Soap Note Template
Progress reports play a pivotal role in physical therapy, offering a snapshot of a patient's journey and progress. At the heart of these reports are Therapeutic Notes, which provide a comprehensive record of each session, ensuring effective communication among healthcare professionals and tracking patient progress. Understanding Therapeutic.
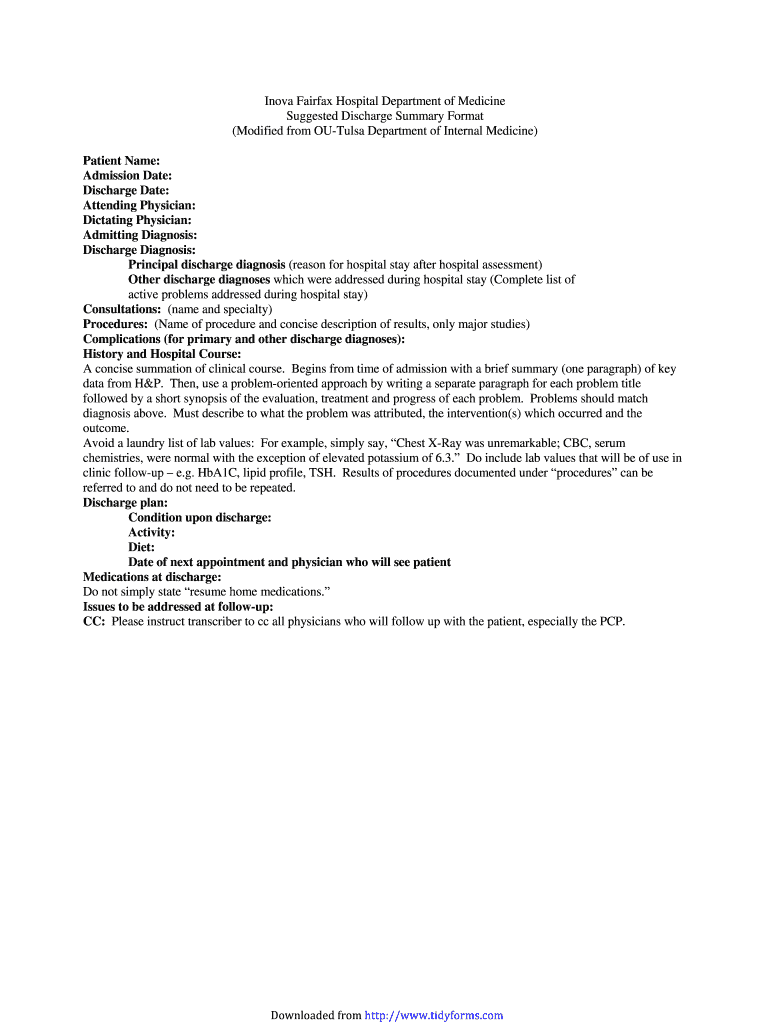
Discharge summary format Fill out & sign online DocHub
Daily Note Assessment & Documentation of Treatment. Progress Note Statements on Goals. Discharge Summary Examples. Goal Setting Template and Examples. The assessment phrases and narrative note examples are enough to save you at least 5 minutes per patient. With 6 patients a day, that saves you 30 minutes each day.

What is the Discharge Summary and Why is it Important
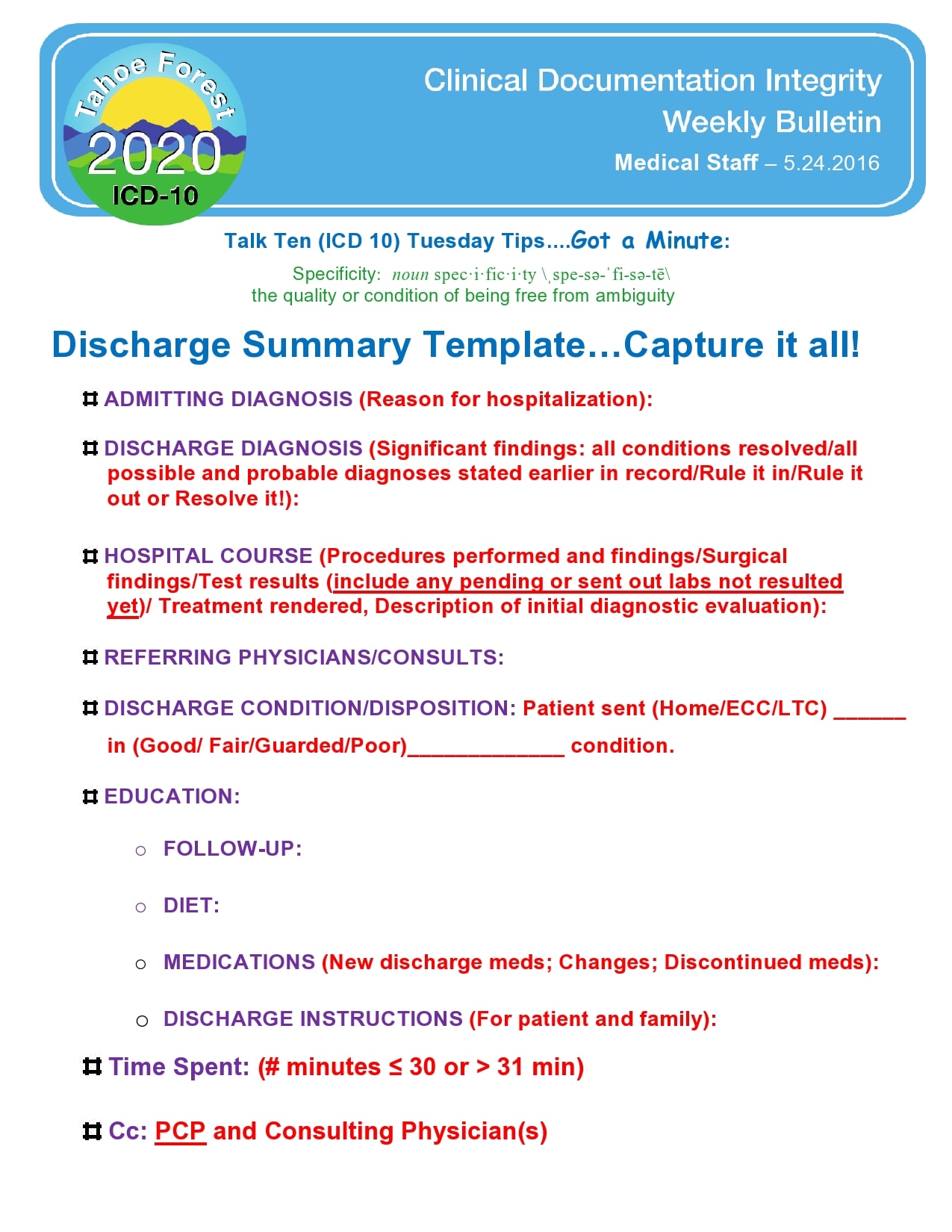
Functionally, a discharge summary (a.k.a. discharge note) is a progress note that covers the reporting period from the last progress report to the date of discharge. The discharge summary is required for each episode of outpatient therapy treatment. Per CMS, "Clinicians should consider the discharge note the last opportunity to justify the.

Physiotherapy Discharge Summary Template Fill Online, Printable
A PT/OT should pen a Progress Report at least once every 10 treatment visits. It's imperative to note that PTAs or OTAs are not authorized to write these reports. Moreover, the time expended in drafting a progress report is non-billable as Medicare deems it encompassed in the treatment time charge. Essential Elements of a Progress Report:

How To Write Therapy Progress Notes 8 Templates & Examples
Physical therapy documentation is an important tool for recording therapy treatments and tracking a patient's progress. It can also be the cause of major headaches, rushed lunch hours, and excessive typing throughout the day. Students and therapists alike have experienced difficulty locating helpful physical therapy documentation examples.