
Free Printable Nursing Handoff Report Template Printable Form
Free downloadable tools to support your work to improve health care quality and safety at every stage — from establishing a project plan and an improvement aim, to understanding a process, to identifying root causes or drivers, to testing changes using PDSA cycles, to implementing and spreading successful improvements, and more. Featured Tools
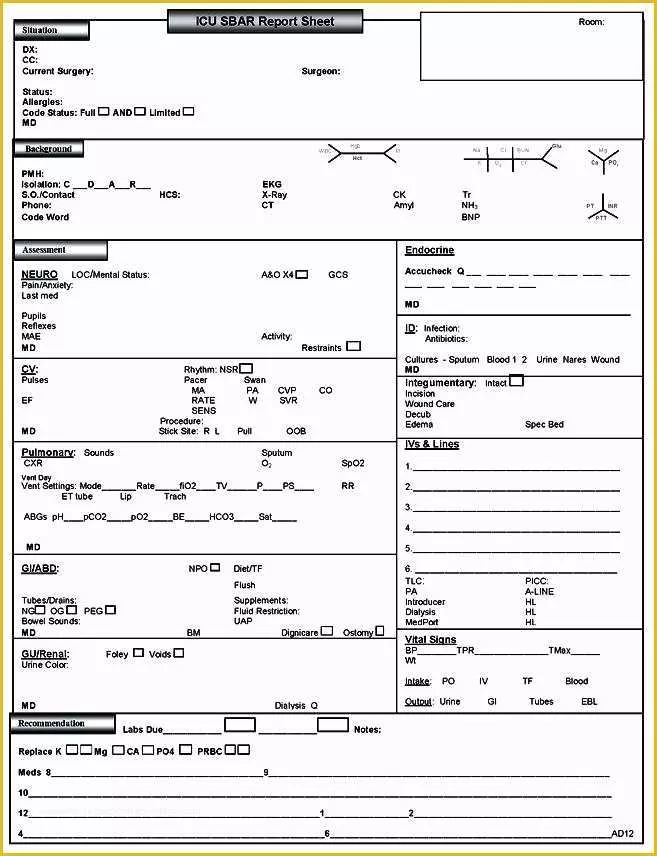
Free Printable Sbar Template Of Nursing Handoff Report Sheet Beautiful
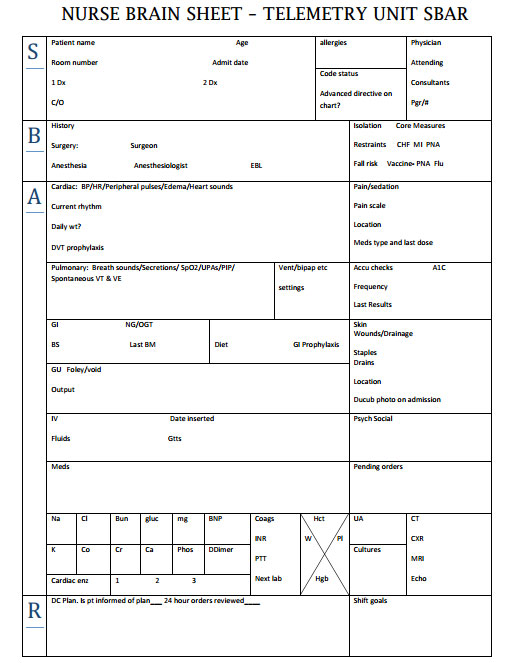
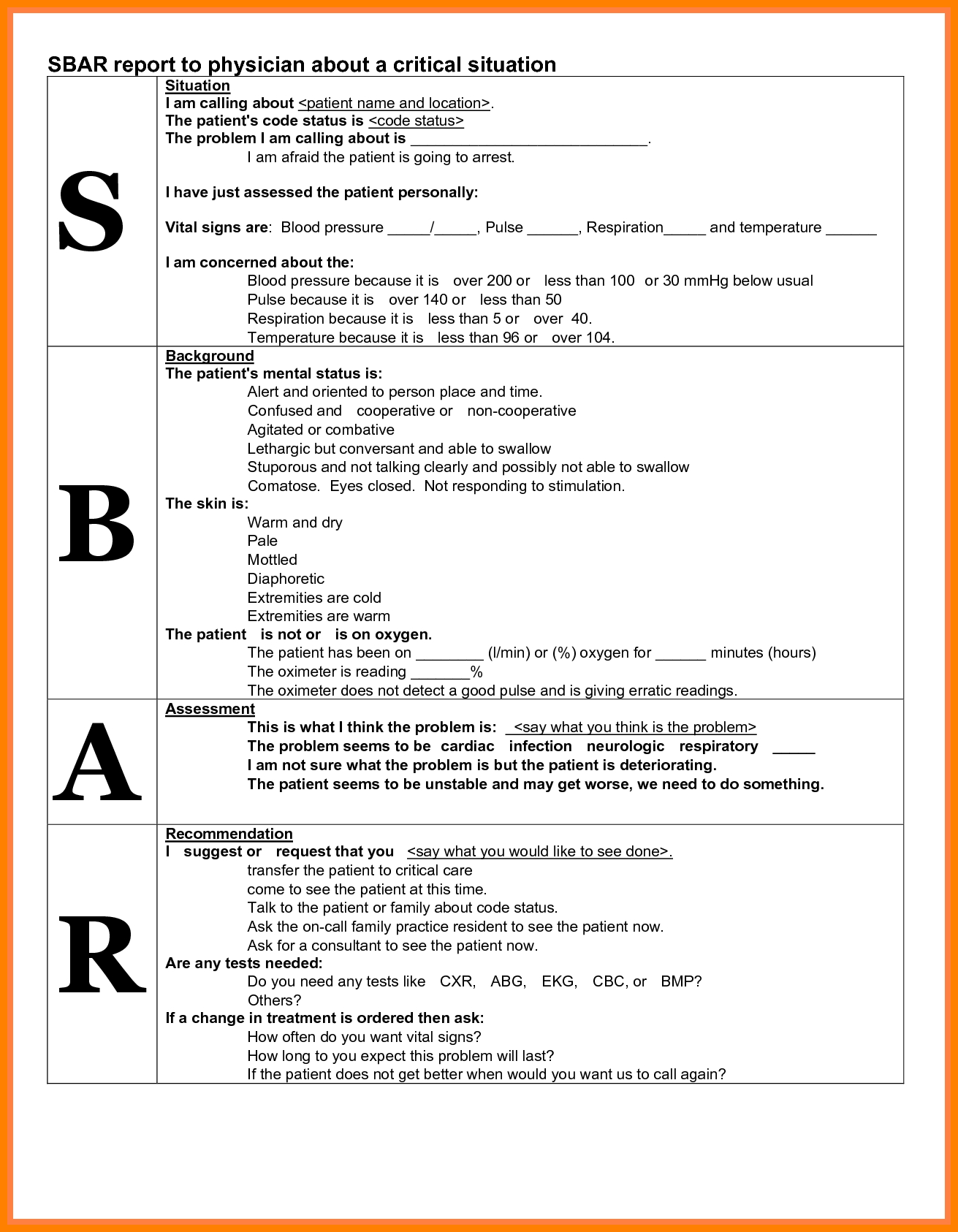
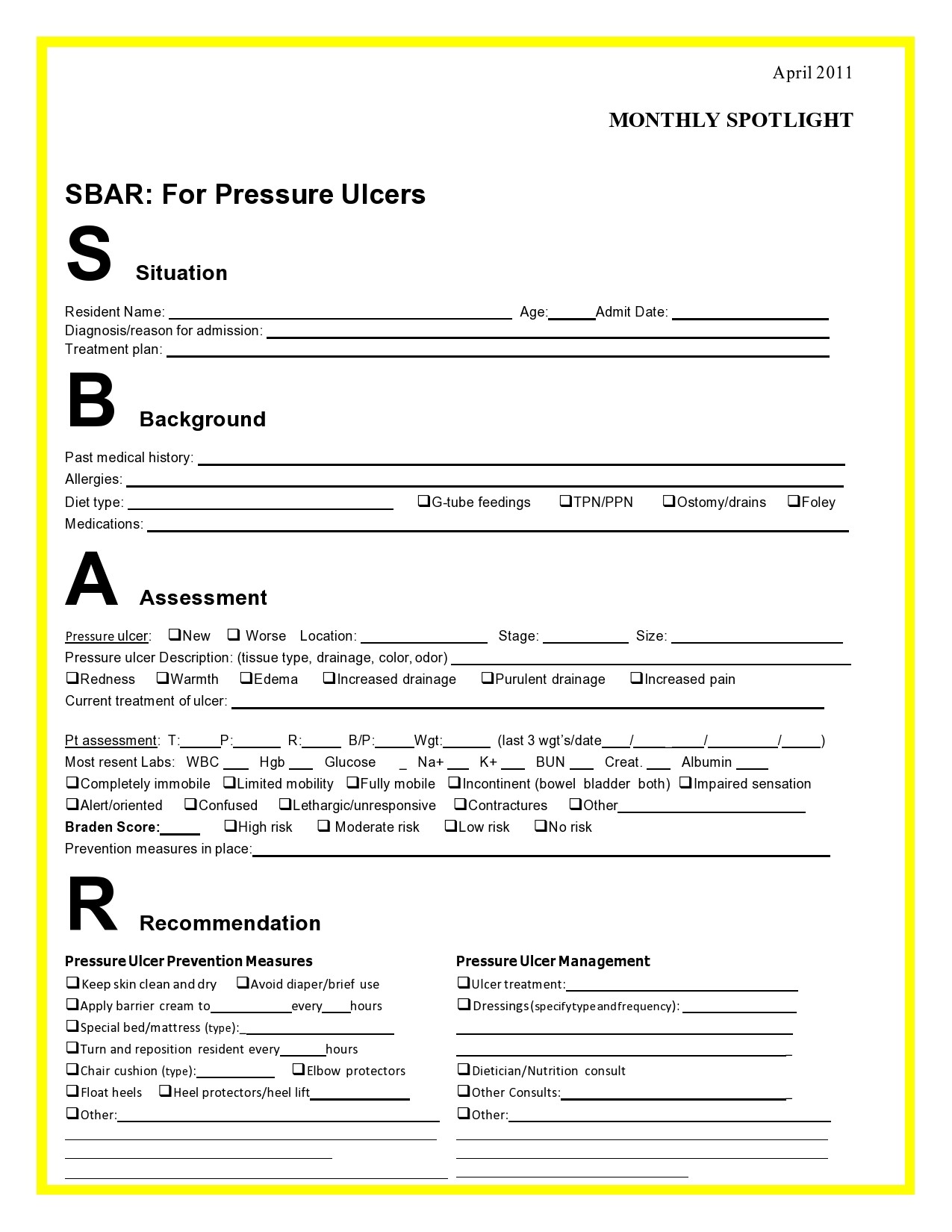
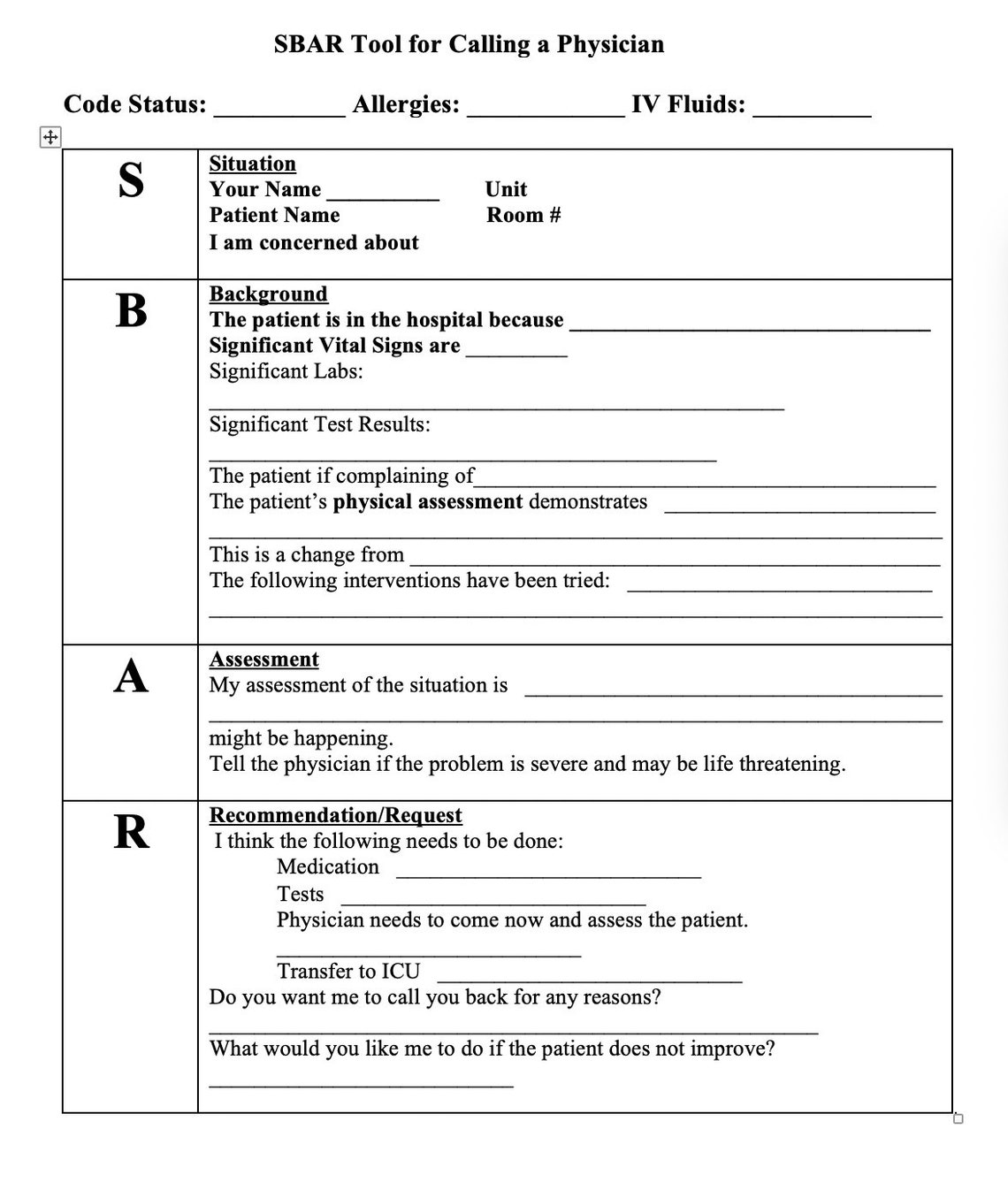
The SBAR (Situation-Background-Assessment-Recommendation) technique provides a framework for communication between members of the health care team about a patient's condition. SBAR is an easy-to-remember, concrete mechanism useful for framing any conversation, especially critical ones, requiring a clinician's immediate attention and action.
Sbar Sheet FREE DOWNLOAD Freemium Templates
SBAR Worksheet: A worksheet/script that a provider can use to organize information in preparation for communicating with a physician about a critically ill patient (includes both an example and a blank SBAR Worksheet template) Both the worksheet and the guidelines use the physician team member as the example; however, they can be adapted for use.

197 best Nursing forms & templates images on Pinterest Nursing
An SBAR report is a tool of communication between members of the healthcare team about a client's condition that follows the SBAR communication technique. SBAR stands for: S ituation B ackground A ssessment R ecommendation What is the purpose of the SBAR technique?

Free download! This is a fullsize SBAR nursing brain report sheet. 1
SBAR ( s ituation, b ackground, a ssessment, r ecommendation) was designed as a communication tool to convey critical information requiring immediate action and advice. It has been adopted widely in healthcare settings as a structured method of communicating important clinical information (e.g. escalation of care, patient handover).

Printable Blank Sbar Template
What is SBAR? SBAR is a standard to communicate medical information. Simply, it improves accuracy and helps to correct dangerous errors. It Stands for: (Situation, Background, Assessment, Recommendation) The above four terms are the key facts. However, all should be conveyed properly.

Sbar Template Word Business Design Layout Templates
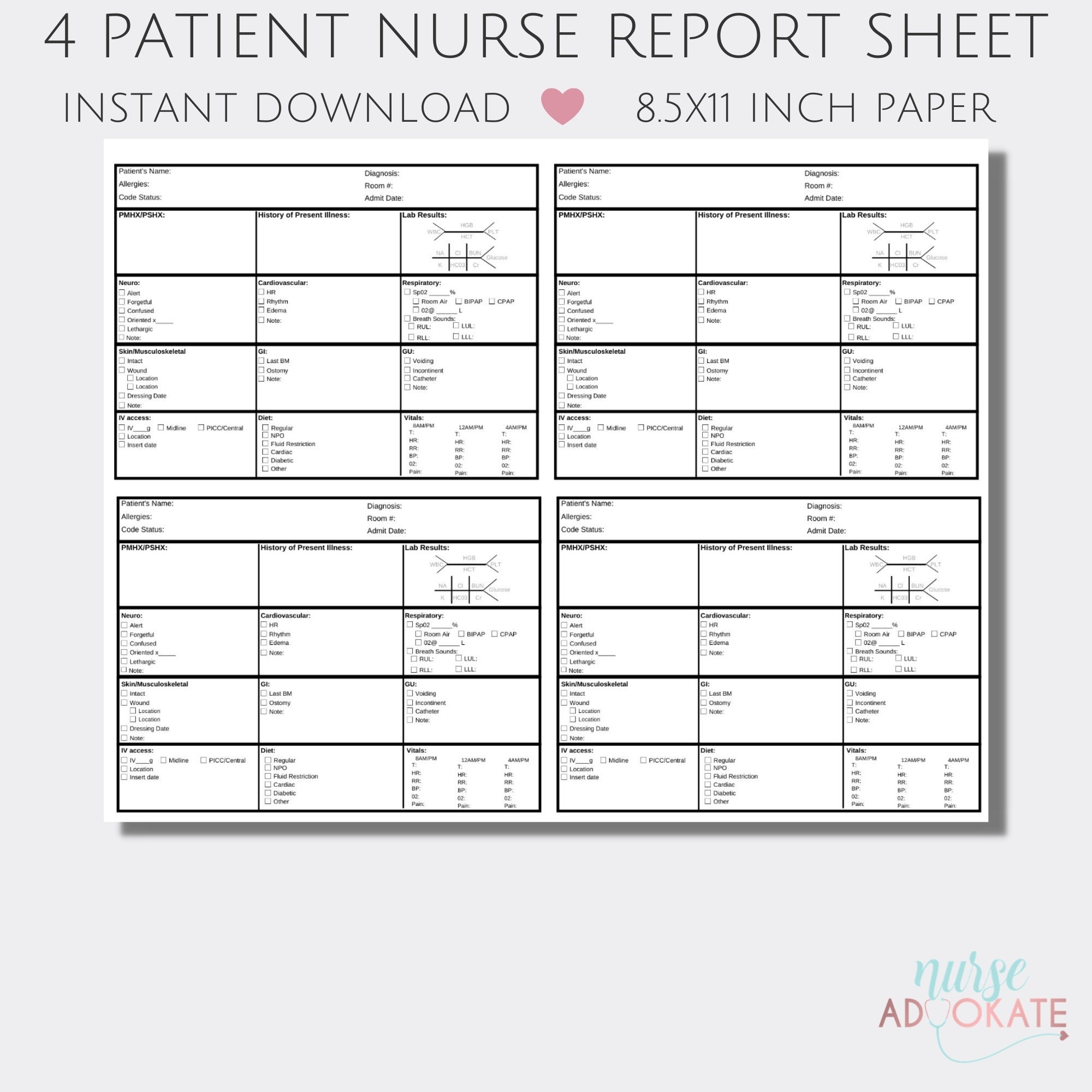
How to Create your SBAR Nurse Report Sheet. You can generate a PDF printout (just like the screenshot above) using the NurseBrain app (available on IOS and Android ). Just open the NurseBrain app, go to your clipboard, swipe right on the patient you want to share and select "Share PDF.". If the incoming nurse already has the NurseBrain app.

Nurses Report Sheet Nurse Report Sheet Nurse Brain Sheet Sbar Images
Safer Care SBAR Situation • Background • Assessment • Recommendation Implementation and Training Guide
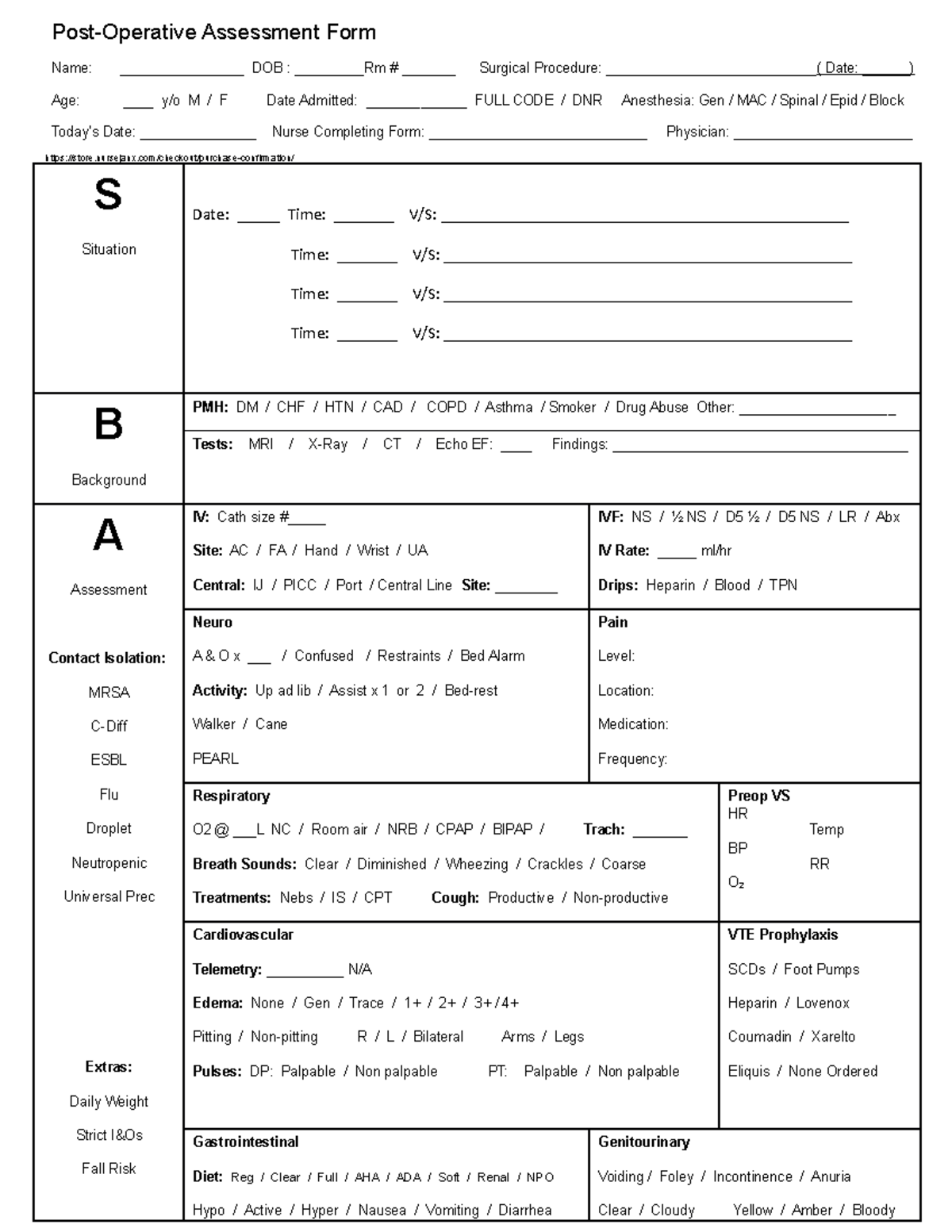
Sbar Fullsize Nursing Report Sheet Op Assessment Studocu Vrogue
An SBAR Report Template serves as a structured framework for facilitating clear and effective communication among healthcare professionals regarding a patient's condition, particularly in situations demanding prompt intervention.
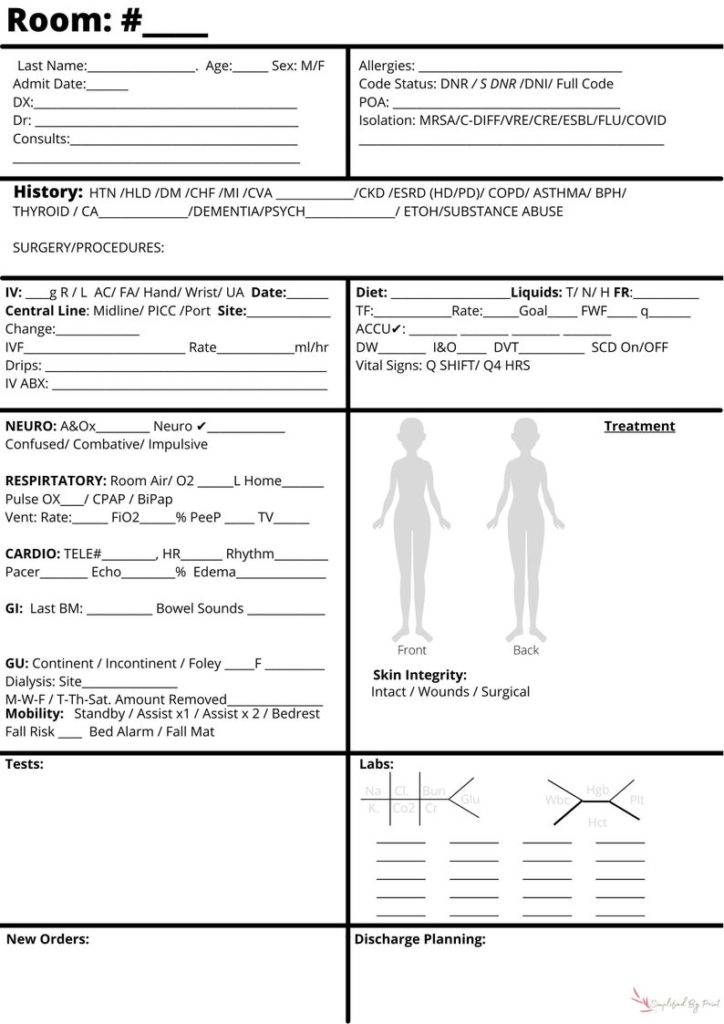
Nursing SBAR Bedside Report Sheet Simplified by Print
SBAR stands for Situation, Background, Assessment, and Recommendation—an effective framework for conveying critical information between healthcare professionals. Our customizable and printable templates provide a structured approach to communicate patient conditions, vital signs, medical history, and recommended actions.

Sbar Nursing Shift Report Form On Sbar Nursing Worksheet Med Surg
15 Excellent SBAR Nursing Examples + How To Use It ☰ Home Degree Entry-Level CNA LPN/LVN ADN BSN Accelerated BSN For Non-Nurses Direct-Entry MSN Non-Nurses Bridge LPN-TO-RN LPN-TO-BSN RN-TO-BSN RN-TO-MSN RN-TO-DNP BSN-TO-DNP Graduate MSN DNP Nurse Practitioner FNP PMHNP NNP - Neonatal NP PNP - Pediatric NP WHNP ACNP AGNP CRNA Ph.D. Programs Careers
Sbar Examples Nurse To Doctor One Checklist That You Should Keep In
SBAR is an easy to remember mechanism that you can use to frame conversations, especially critical ones, requiring a clinician's immediate attention and action. It enables you to clarify what information should be communicated between members of the team, and how. It can also help you to develop teamwork and foster a culture of patient safety.
nursing report sheet b etsy 4 patient night shift report sheet nurses
Download this free SBAR template to efficiently document the Situation, Background, Assessment, and Recommendation about a particular patient or case. Using this template, be able to completely provide information to help ensure continuity of patient care by doing the following:
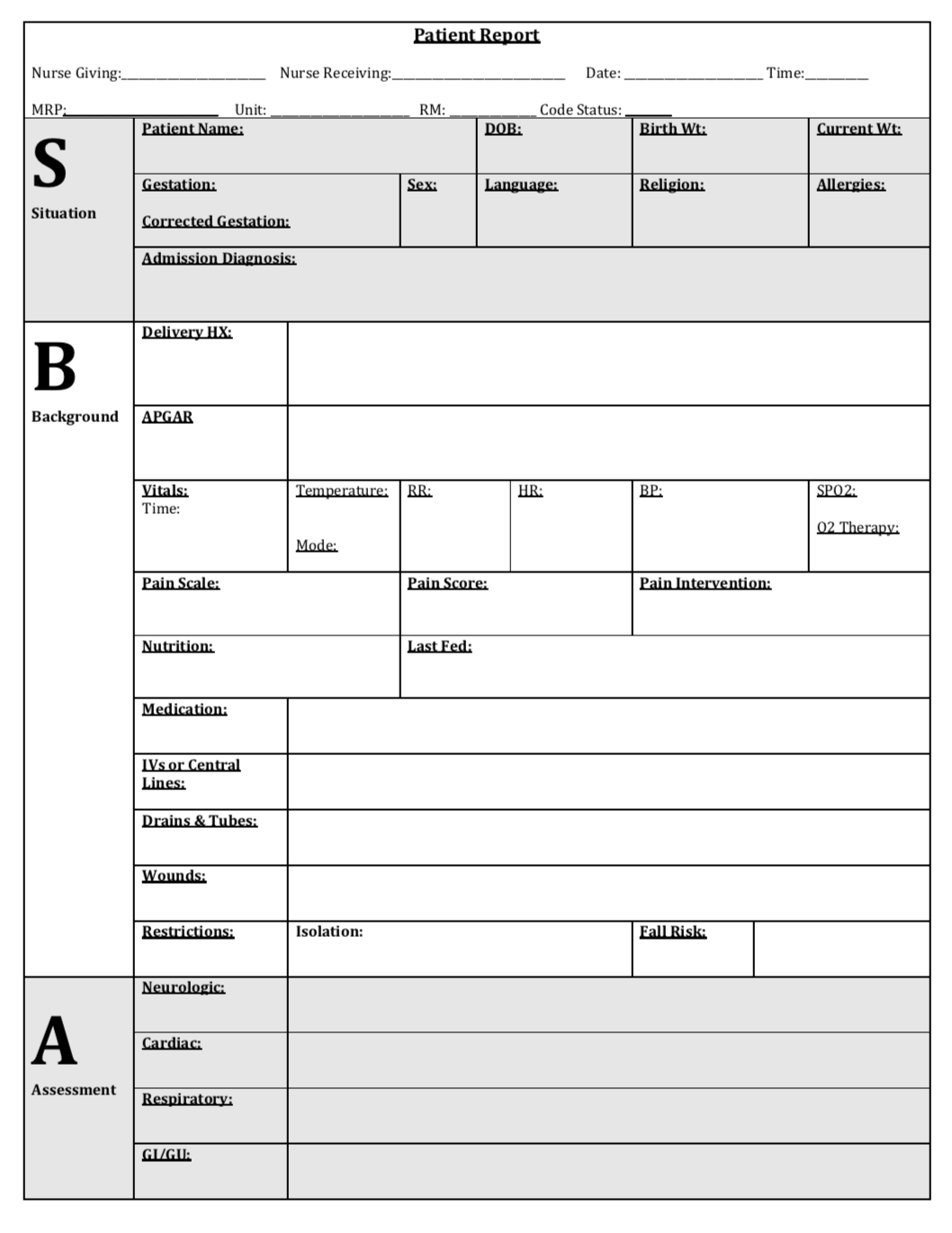
SBAR Patient Report Newborn Simulation
SBAR, which stands for Situation, Background, Assessment, and Recommendation (or Request), is a structured communication framework that can help teams share information about the condition of a patient or team member or about another issue your team needs to address. In phrasing a conversation with another team member, consider the following:
Sbar Report Template
SBAR Worksheet ("SBAR report to physician about a critical situation"): A worksheet/script that a provider can use to organize information in preparation for communicating with a physician about a critically ill patient
Printable Nursing Handoff Report Template
The SBAR (Situation, Background, Assessment, Recommendation) tool is used by all nursing fields within primary and secondary healthcare environments to aid patient safety ( NHS Improvement, 2018 ). Acts of communication through handovers, ward rounds, shift exchanges and team meetings are examples of when information is exchanged between nurses.